Menière's disease
Menière's disease is a chronic and often debilitating disorder of the inner ear. The inner ear is a crucial part of our anatomy responsible for both hearing and balance. While there is currently no known cure for Menière's disease, understanding its complexities, recognizing its symptoms, and exploring effective management strategies can significantly improve quality of life for those affected.
Read on for an overview of Menière's disease, its symptoms, diagnostic criteria, and the role of vestibular rehabilitation physiotherapy.
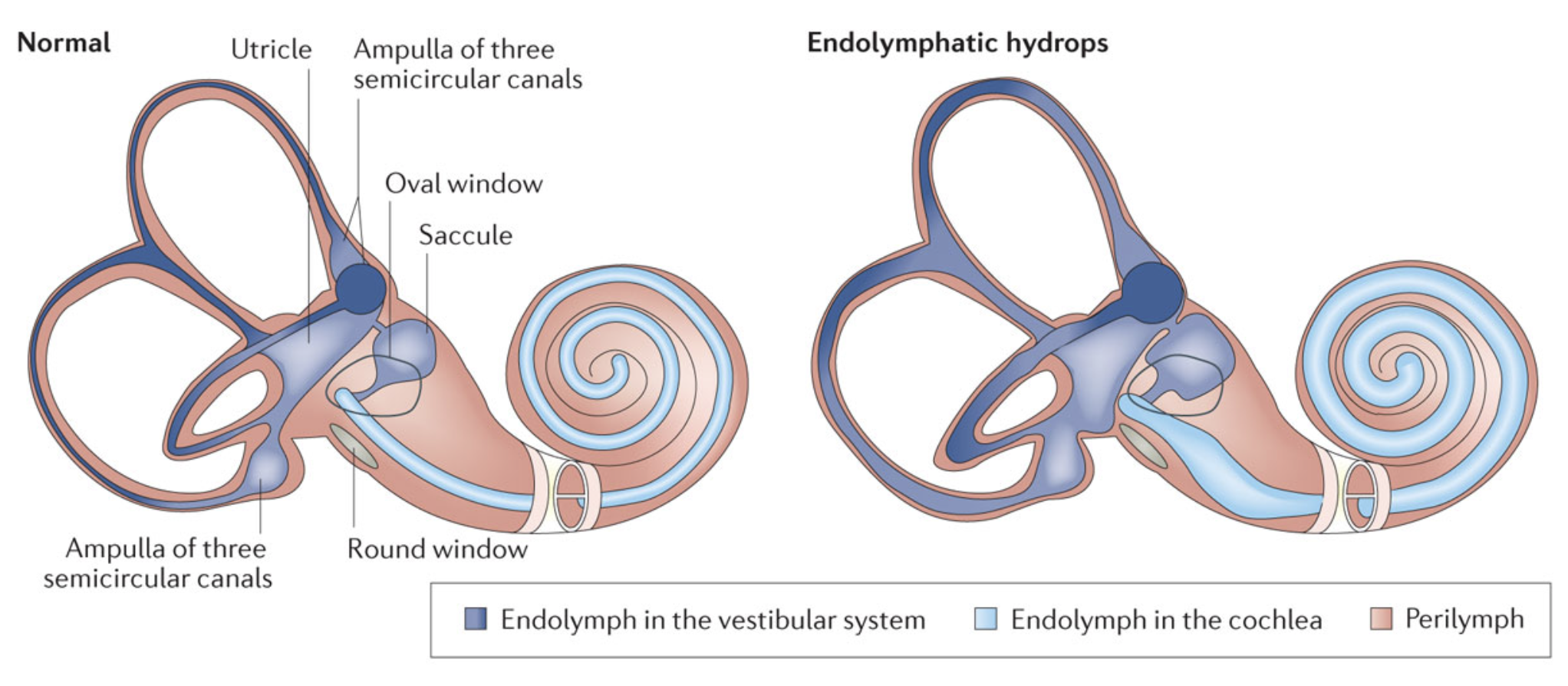
Image from Nakasima et al. 2016
Endolymphatic hydrops & Menière's
Menière's disease is believed to be caused by endolymphatic hydrops, which involves an abnormally large accumulation of endolymph fluid within the inner ear's delicate membranes. This fluid imbalance is thought to interfere with the normal signals transmitted from the inner ear to the brain, which leads to the characteristic symptoms of the disease. While endolymphatic hydrops is observed in individuals diagnosed with Menière's disease, its presence alone does not always result in the full spectrum of symptoms. This suggests that other factors, possibly subtle biochemical or structural changes within the inner ear, may also contribute to how this condition manifests. It is thought that microvascular dysfunction and/or immune system dysregulation are potential mechanisms that contribute to development of Menière's. In Menière's disease, the endolymphatic hydrops is idiopathic - meaning it has an unknown cause. This is sometimes referred to as ‘primary endolymphatic hydrops’.
Endolymphatic hydrops can also occur in response to an underlying disease, infection, or injury. This is sometimes referred to as ‘secondary endolymphatic hydrops’. Potential causes include autoimmune or inflammatory disorders, vestibular neuritis or labyrinthitis, head trauma, or inner ear surgery (e.g. cochlear implantation, stapedectomy for otosclerosis). In some cases, endolymphatic hydrops can occur in a delayed manner after sudden sensorineural hearing loss (SSNHL).
Symptoms of Menière's disease
Menière's disease typically affects adults between 40 and 60 years of age, though it can occur at any age.
Menière's disease is defined by four primary symptoms:
Episodic Vertigo: This is typically the most disruptive symptom, usually described as a severe spinning sensation. Vertigo attacks often begin without warning and are frequently accompanied by nausea, vomiting, and significant imbalance. These episodes typically last between 20 minutes and 12 hours. The frequency of attacks can vary widely both between and within individuals, from multiple times a week to long periods of remission.
Fluctuating Hearing Loss: Individuals with Menière's disease often experience hearing loss, particularly in the low to medium frequencies. This hearing loss can come and go, especially in the early stages of the disease. Over time, hearing impairment may become more pronounced and permanent.
Tinnitus: This symptom is a perception of sound in the ear when no external sound is present. It is often described as ringing, buzzing, roaring, whistling, or hissing. Like hearing loss, tinnitus can fluctuate in intensity or become persistent over time.
Aural Fullness or Pressure: Many individuals report a sensation of pressure, congestion, or fullness in the affected ear, often preceding or accompanying a vertigo attack.
The pattern of Menière's symptoms can be unpredictable and can evolve over time. Attacks are sometimes preceded by warning signs, such as a feeling of imbalance, increased ear pressure, or a change in the intensity of hearing loss or tinnitus. In the early stages, vertigo attacks are often sudden and intense. In between the acute episodes of vertigo, some individuals may experience complete resolution of symptoms and feel entirely normal between spells. For others, the periods between attacks are not entirely symptom-free, with more persistent symptoms that may include fatigue, oscillopsia, and/or imbalance. Some individuals experience sudden and unexpected falls known as "drop attacks".
In later stages of Menière's, the symptom presentation often changes. Hearing loss may become more significant and permanent. Tinnitus and aural fullness may also become stronger and more constant. The intense vertigo attacks may lessen in frequency or severity, but they can be replaced by more persistent vision and balance issues.
This evolution in symptoms means that early management often focuses on controlling acute attacks of vertigo, but as the condition advances the focus shifts towards addressing chronic imbalance and hearing loss. Vestibular rehabilitation can have an important role in supporting long-term function and well-being.
Menière's diagnostic criteria
Diagnosing Menière's disease is a clinical process, relying on a careful and holistic evaluation of a patient's symptoms, medical history, clinical examination, and specific findings on audio-vestibular testing, rather than a single definitive test. Several other conditions can mimic the symptoms of Menière's, such as vestibular migraine, transient ischemic attacks (TIAs), tumors, vestibular neuritis, or recurrent vestibulopathy. Menière's also commonly co-occurs with other vestibular disorders, such as BPPV and PPPD. A thorough evaluation is essential to ensure an accurate diagnosis.
To standardize diagnosis globally, the Bárány Society, an international multidisciplinary society dedicated to vestibular research, established specific diagnostic criteria in 2015. These criteria classify Menière's disease into "Definite" and "Probable" categories, based on the presence and characteristics of key symptoms.
Definite Menière's Disease
Two or more spontaneous episodes of vertigo, each lasting 20 minutes to 12 hours.
Low to medium frequency sensorineural hearing loss in one ear on at least one occasion before, during or after a vertigo episode, documented on audiogram.
Fluctuating aural symptoms (hearing, tinnitus or fullness) in the affected ear.
Not better accounted for by another vestibular diagnosis.
Probable Menière's Disease
Two or more episodes of vertigo or dizziness, each lasting 20 minutes to 24 hours.
Fluctuating aural symptoms (hearing, tinnitus or fullness) in the affected ear.
Not better accounted for by another vestibular diagnosis.
Diagnostic tests for Menière's
While the Bárány Society's criteria provide a solid framework for diagnosing Menière's Disease, clinicians often rely on specialized tests and imaging techniques to support the diagnosis and rule out other conditions.
Audio-vestibular testing
Videonystagmography (VNG) and Caloric Testing: VNG records eye movements (nystagmus) during various maneuvers to evaluate the function of the balance organs in the inner ear. The caloric test, a component of VNG, involves introducing warm and cool air or water into the ear canal. This stimulates the inner ear and generates a specific eye movement response. In Menière's disease, caloric testing often reveals reduced function in the affected ear, indicating a unilateral vestibular weakness.
Vestibular Evoked Myogenic Potentials (VEMP): VEMPs measure the integrity of specific vestibular pathways. Cervical VEMPs (cVEMPs) assess the saccule and inferior vestibular nerve, while ocular VEMPs (oVEMPs) assess the utricle and superior vestibular nerve. In Menière's, VEMPs may show reduced or absent responses in the affected ear.
Video Head Impulse Test (vHIT): The vHIT evaluates the function of all six semicircular canals (the parts of the inner ear that detect head rotation). During the test, you fix your gaze on a target while the clinician rapidly moves your head. High-speed video measures your eye movements. Where the caloric test assesses low-frequency vestibular function, vHIT evaluates high-frequency function and the vestibulo-ocular reflex. The VOR may be more subtly affected in early Meniere's or between attacks, and may be more significantly affected in later stages.
Electrocochleography (ECochG): This test measures the electrical potentials generated by the hearing portion of the inner ear (cochlea) in response to sound. It is a test that can detect endolymphatic hydrops – the excess fluid in the inner ear that is believed to be the underlying pathology of Menière's disease. An increased ratio between two specific electrical potentials (SP/AP ratio) is a common finding in Menière's and suggests the presence of hydrops.
Audiogram (Hearing Test) and Low-Frequency Hearing Loss: An audiogram is a fundamental test that measures your hearing sensitivity across different frequencies. In Menière's, a characteristic finding is a fluctuating low-to-medium frequency sensorineural hearing loss in the affected ear. This means that sounds in the lower pitch range (like deep voices or bass notes) are harder to hear. This hearing deficit can come and go, and is often present during or after vertigo attacks. Over time, the hearing loss may progress to a permanent low frequency hearing loss, or may affect more frequencies with a ‘tent-like’ pattern of loss at both low and high frequencies.
Advanced imaging to visualize hydrops
Delayed Contrast MRI of the Inner Ear: In recent years, advances in MRI technology have made it possible to directly visualize endolymphatic hydrops. This specialized MRI technique involves injecting a contrast agent (gadolinium) intravenously, then waiting several hours (typically 4 hours) before performing the scan. This delay allows the contrast agent to diffuse into the perilymphatic fluid but not into the endolymphatic fluid. The resulting images can then show the distinction between the two fluid compartments, revealing areas where the endolymphatic sac is distended due to hydrops. This direct visualization can support a Menière's diagnosis, especially in atypical cases, by providing objective evidence of the underlying pathology. It is important to note that Menière's is a clinically defined syndrome, diagnosed by a pattern of symptoms and not solely by the detection of hydrops through imaging.
These diagnostic tools, when combined with a thorough clinical history and physical examination, help clinicians piece together the complete picture, leading to a more accurate diagnosis and a tailored management plan.
Treatment for Menière's disease
While there is no cure for Menière's disease, a variety of treatments and management strategies can significantly improve symptoms, reduce the frequency and severity of vertigo attacks, and improve overall quality of life. Management typically involves a combination of acute attack management, longer-term preventative measures, psychological support, and vestibular rehabilitation physiotherapy.
Acute attack management
During a severe vertigo attack, the primary goal is to reduce the intense spinning sensation, nausea, and vomiting. Medications commonly prescribed for this purpose include sedatives (e.g. lorazepam), and anti-nausea drugs (e.g. Gravol). These medications help to calm the vestibular system and manage associated symptoms, to provide some relief during an episode.
Preventing attacks with medications, injections, and lifestyle changes
For longer-term management, conservative approaches are often the first line of treatment.
Lifestyle changes are often recommended. One strategy is a reduced-sodium diet, typically aiming for less than 1500mg of sodium per day. Limiting salt intake may help to reduce the fluid pressure within the inner ear, which could decrease the frequency and severity of attacks. Patients are often advised to avoid processed foods, cured meats, and many packaged snack foods to help reduce sodium intake. Other lifestyle modifications may include avoiding caffeine, alcohol, and tobacco, as some people find these can be triggers or worsen symptoms. Managing stress effectively and ensuring adequate sleep are also important, as stress and fatigue can exacerbate symptoms.
Diuretics (water pills) may be prescribed to help reduce overall fluid retention in the body, which could ease fluid pressure in the inner ear.
Betahistine (Serc) may be prescribed, although its mechanism of action is not entirely clear and there is conflicting evidence on its clinical efficacy. This medication is thought to increase histamine and improve circulation in the inner ear. This is usually taken daily as a preventative, to try to decrease the frequency and intensity of vertigo attacks.
Intratympanic corticosteroid injections may also be used to control vertigo attacks. A topical anesthetic (e.g. lidocaine-prilocaine) is applied to the tympanic membrane (eardrum), then a needle is used to inject steroids (e.g. dexamethasone) through the tympanic membrane into the middle ear space. A series of injections is often performed, for example once per week for 3 to 6 weeks. Injections may then be performed on an as-needed basis.
Vestibular rehabilitation physiotherapy for Menierè’s
While medications and dietary changes focus on managing fluid balance and acute symptoms, vestibular rehabilitation therapy (VRT) is an exercise-based approach to improve balance and reduce dizziness, particularly in the periods between acute attacks. Vestibular rehab can enhance your ability to cope with the imbalance, dizziness, and unsteadiness that often persist as the disease progresses.
The fundamental principle behind vestibular rehab is neuroplasticity - our brain's ability to adapt and compensate for inner ear balance deficits. When the inner ear is affected by Menière's disease, the brain receives inconsistent or inaccurate signals about head position and movement from the vestibular system. Vestibular rehab works by systematically challenging the balance system, encouraging the brain to retrain itself to process vestibular signals more effectively and to appropriately use other senses such as vision and proprioception (body's sense of position), in order to improve stability.
The goals of vestibular rehab are tailored to your individual needs and could include:
Improve Gaze Stability: VOR adaptation or gaze stability exercises involve head and eye movements, and help improve the ability to keep vision clear during head motion.
Enhance Postural Stability: Balance exercises help improve overall steadiness and reduce the risk of falls. These are sometimes performed on unstable surfaces, with eyes closed, and/or with head movements.
Decrease Dizziness: Through a process called habituation, patients gradually and repeatedly expose themselves to movements or environments that provoke dizziness. This allows the brain to learn to cope with these sensations through desensitization, reducing intensity and frequency of motion and/or visually provoked dizziness over time.
Improve Activities of Daily Living: Vestibular rehab helps individuals regain confidence and independence in everyday tasks by addressing balance deficits and supporting functional goal setting.
A customized vestibular rehab program supported by a physiotherapist with advanced training is more effective than generic exercises because it directly targets the specific movements and situations that provoke dizziness for an individual. These exercises are carefully progressed as your symptoms and abilities improve. Many people initially find vestibular rehab exercises to be challenging as they intentionally provoke symptoms in a controlled way to facilitate adaptation - this is a positive sign that the brain is being challenged and is learning to compensate.
It is important to understand that vestibular rehab is not designed to treat acute vertigo attacks caused by Meniere’s, but rather the persistent dizziness and imbalance that occur between these episodes, or the chronic imbalance and gaze stability deficits that may develop in later stages of the disease.
For vestibular rehab to be most effective, patients should be motivated and have realistic expectations. It is also important to note that regular use of certain medicines, particularly vestibular sedatives, can hinder the brain's ability to adapt during vestibular rehab so medication regimens may need to be adjusted. A multidisciplinary team approach provides comprehensive care, and includes physiotherapists, ENT physicians, audiologists, and psychotherapy. Treatment typically requires medical management and mental health support alongside rehabilitation efforts.
More invasive treatments
For severe or refractory cases where conservative medical treatments and vestibular rehab do not adequately control symptoms, more invasive options may be considered. These include intratympanic injections of ototoxic medications like gentamicin (which damages the vestibular organs in the inner ear to limit vertigo attacks), or surgical procedures aimed at relieving inner ear pressure or stopping signals from the affected ear being sent to the brain. Surgical procedures include endolymphatic sac decompression, tenotomy of the tendon of the stapedius and tensor tympani muscles, vestibular nerve section, or labyrinthectomy. Procedures such as gentamicin injections or surgeries can stop attacks of vertigo, however they lead to permanent vestibular loss which can result in imbalance and oscillopsia. Vestibular rehabilitation may be required to help improve symptoms and facilitate compensation for the resulting loss of vestibular function.
These invasive options are typically considered as last resorts due to potential risks, including further hearing loss. Also, approximately 13% of people with Menière's disease initially affecting one ear (unilateral Menière's) go on to develop Menière's in the other ear as well (bilateral Menière's). When an ablative procedure may lead to a complete loss of hearing and balance in one ear, it can lead to significant functional impairment if the other “good” ear later develops endolymphatic hydrops.
Final thoughts and next steps
Menière's disease is a complex inner ear disorder characterized by fluctuating symptoms, including episodic vertigo, hearing loss, tinnitus, and aural fullness. While its exact cause remains unknown, and there is no definitive cure, significant progress has been made in understanding its diagnosis and management. Coping with Menière's disease involves a combination of medical management, rehabilitation, and proactive self-care strategies.
While the journey with Menière's disease can be unpredictable, a comprehensive and individualized treatment plan with a collaborative healthcare team, can help manage symptoms and improve quality of life. Effective management of Menière's disease relies on a multifaceted approach that combines acute symptom relief, medical management to control attacks, active rehabilitation therapies, and support from family, friends and trained professionals. Vestibular rehabilitation physiotherapy uses your brain's neuroplasticity to improve balance, reduce chronic dizziness, and enhance function between attacks.
Ready to start vestibular rehab? Book an appointment with our experienced team.
-
-
Nakashima, T., Pyykkö, I., Arroll, M. et al. Meniere's disease. Nat Rev Dis Primers 2, 16028 (2016). [link]
Ferster APO, Cureoglu S, Keskin N, Paparella MM, Isildak H. Secondary Endolymphatic Hydrops. Otol Neurotol. 2017;38(5):774-779. [link]
Venkatasamy A, Péporté ARJ. Secondary endolymphatic hydrops: a clinical and literature overview. Front Neurol. 2025;15. [link]
Lopez-Escamez JA, Carey J, Chung WH, et al. Diagnostic criteria for Menière’s disease. VES. 2015;25(1):1-7. [link]
Young AS, Nham B, Bradshaw AP, et al. Clinical, oculographic and vestibular test characteristics of Ménière’s disease. J Neurol. 2022;269(4):1927-1944. [link]
Lee SU, Park E, Kim HJ, Choi JY, Kim JS. Evolution of Vestibular Findings During and Between the Attacks of Meniere Disease: Update. Neur Clin Pract. 2024;14(2):e200235. [link]
Patel M. Intratympanic corticosteroids in Ménière's disease: A mini-review. J Otol. 2017;12(3):117-124. [link]
Hudson TJ, Tan LSH, Phillips V, Muzaffar J, Bance M. Long-Term Risk of Progression From Unilateral to Bilateral Méniere’s Disease: A Systematic Review and Meta-Analysis. Otol Neurotol. 2025;46(5):485-493. [link]
Yuan VG, Xia A, Santa Maria PL. Immunological mechanisms in Meniere’s disease. Front Immunol. 2025;16:1639916. [link]