Sleep and vestibular disorders
Healthy sleep is important, but sleep problems are common with vestibular disorders and poor sleep can worsen symptoms like dizziness and imbalance. Read on for information about the relationship between sleep issues and vestibular dysfunction, why sleep is important, and tips for improving your sleep.
Healthy sleep
Sleep is restorative! Growth hormone release, protein synthesis, and tissue repair occur during sleep, and these functions are important for healing and recovery in our bodies. There is also a connection between sleep and brain plasticity. Brain plasticity, also known as neuroplasticity, is the ability of the structure and organization of our brain to change. Neuroplasticity is the rewiring and growth of our brain connections, and it is important for learning, memory, and recovery from brain injury or vestibular loss. Sleep is important for our brain to develop new connections and pathways. Sleep is also important for consolidating memory.
Most adults need 7 to 9 hours of sleep per night, though some people need more or less.
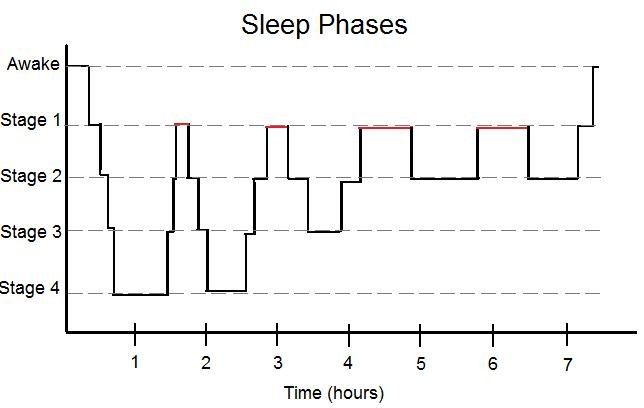
There are two types of sleep - rapid eye movement (REM) sleep and non-REM sleep. We move through different stages or phases of sleep:
Stage 1 - non-REM
“Dozing off”
Light sleep that occurs when going from wakefulness to sleep
Stage 2 - non-REM
Light sleep where brain waves slow (though there are short bursts of brain activity)
Body temperature drops, muscles relax, heart rate and breathing slow down
Stage 3 - non-REM
“Deep sleep”
Brain waves become even slower (delta or slow waves)
Muscles relax even more, and heart rate and breathing slow down further
Important for restorative sleep and body recovery
Stage 4 - REM
When most of your dreams occur
Eyes move quickly underneath closed eyelids
Brain wave activity increases
Breathing, heart rate, and blood pressure increase
Muscles are temporarily paralyzed so you do not act out dreams
Important for cognitive functions
We transition through these stages of sleep during the night - this is our sleep cycle. We go through 4 to 6 sleep cycles per night, though sleep cycles vary from night to night and from person to person. On average each sleep cycle lasts 90 minutes, but our first sleep cycle of the night is usually the shortest and later cycles are typically longer.
Sleep, fatigue, and vestibular dysfunction
Sleep problems can mean having trouble falling asleep, having trouble staying asleep (i.e. waking up during the night), waking up too early in the morning, having unrefreshing or restless sleep, or sleeping too much.
Sleep disturbance is common with vestibular disorders. People with vertigo, imbalance, or dizziness due to a vestibular problem have a higher risk of both sleeping too little and sleeping too much. Sleep disturbance is common in people experiencing dizziness, and seems to be particularly common in people with vestibular migraine, Meniere’s Disease, and Persistent Postural Perceptual Dizziness (PPPD). Some research has found that people with vestibular migraine are more likely to have poor sleep quality, have decreased sleep efficiency (the percentage of time actually asleep while in bed), have reduced REM and slow wave sleep, have a higher proportion of light sleep, take longer to fall asleep, and wake up more frequently during the night.
One study found that people with chronic unilateral vestibular hypofunction (i.e. after having vestibular neuritis or labyrinthitis) spent less time sleeping and took more time to fall asleep. Research has also observed that people with peripheral vestibular dysfunction and poor sleep quality demonstrate worse balance and higher risk of falls. Sleep disruption can occur with Benign Paroxysmal Positional Vertigo (BPPV) as symptoms can be triggered when moving in bed, causing frequent awakenings during the night. People with obstructive sleep apnea appear to have a higher incidence of peripheral vestibular disorders.
Sleep disturbance is also a common symptom after brain injury and concussion. This includes problems falling asleep, problems staying asleep, and poor sleep quality. Excessive sleepiness during the daytime, increased need for sleep, and changes in the sleep-wake cycle are also common symptoms after brain injury. After mild traumatic brain injury (mTBI) or concussion, it is very common to sleep a lot in the first couple of weeks after the injury, and then to develop insomnia.
Changes in your activity and sleep routines are common when you have experienced a vestibular disorder, and also after concussion or other brain injury. This often happens when you are not able to participate in your usual daily activities. Decreased activity levels and disruption in your daily schedule can have a negative impact on your sleep.
Fatigue is a common issue with both brain injury and vestibular disorders. Physical and mental fatigue are common after brain injury - it takes more effort to perform your usual activities. When your vestibular system is not working correctly, your brain needs to work harder to interpret sensory signals, maintain your balance, and keep your eyes focused (due to vestibulo-ocular reflex loss) which takes much more energy and can lead to feeling more easily fatigued. Poor sleep can worsen problems with fatigue. Other symptoms like pain, stress, and low mood can also contribute to fatigue.
Why sleep is important for health and recovery
Sleep deprivation can amplify your symptoms. Insomnia can make you more sensitive to symptoms and their triggers:
Poor sleep can be a symptom trigger in vestibular migraine
Poor sleep can aggravate persistent post-concussion symptoms
Poor sleep may be associated with increased fall risk
Poor sleep is a risk factor for anxiety and depression
Sleep deprivation has a negative impact on postural stability (your ability to stay balanced)
Sleep deprivation affects our attention, making it more difficult to concentrate, learn, and remember
Not getting enough sleep is also linked to other health issues like weight gain, type II diabetes, hypertension, anxiety and mood disorders, and lower life expectancy.
How to improve your sleep
Keep a regular bedtime and wake time - Try to maintain a steady schedule - go to bed and get up at the same time each day. This can take time to establish, so stick with it!
Optimize your sleep environment - Keep your bedroom dark, cool, and comfortable.
Keep a relaxing routine around bedtime - Plan for a calming transition to bedtime, and keep a consistent routine that tells your brain it is time to sleep. Dim the lights. Minimize screen time before bed and put your devices on ‘do not disturb’ mode. If thoughts keep you awake, set aside some dedicated ‘planning’ or ‘worry’ time to write down your to-do list. Try winding down with some gentle yoga or stretching.
If you can’t fall asleep after about 20 minutes, keep the lights dim but get up and do something calming - this is to associate being in bed with sleep and not with restless wakefulness.
Mindful breathing, guided meditation, or progressive muscle relaxation can help you to relax before bed. There are many different apps, audio and video recordings, and online resources you can try. Here are some links to examples:
Minimize or avoid napping during the day - We need to build up our ‘drive to sleep’ and napping can interfere with this. Napping for too long or too close to bedtime can affect your ability to fall asleep at night. Avoid napping later in the afternoon or evening, and keep naps short - about 20 minutes.
Don’t watch the clock - if you wake during the night, resist the impulse to check the time.
Get exercise regularly, but not right before bedtime.
Spend some time outdoors during the day - getting some exposure to sunlight, particularly in the morning, can help reset your body’s “internal clock” sleep-wake cycle.
Try using white noise if tinnitus or sounds in your environment disturb sleep.
Minimize or avoid caffeine - if you have problems sleeping try to avoid consuming caffeine after 1pm. Caffeine is a stimulant and remains in your system for longer than you think, as the half life of caffeine is about 5 hours (the half life is the time it takes for a substance in your body to decrease to half the original amount). Caffeine can make it more difficult to fall asleep, can reduce your total sleep time, and can decrease the amount of deep sleep you get.
Minimize or avoid alcohol before bedtime - alcohol disrupts your sleep cycle and causes changes in your REM sleep stages.
CBT for insomnia (CBTi or CBT-I) is an evidence-based treatment that research has found to be more effective and safer than sleeping pills. You can find more information on CBTi here.
Positioning for sleep if you have BPPV - ideally we would resolve your BPPV with treatment maneuvers! If you are actively having spells of positional vertigo and these are interrupting your sleep, try temporarily sleeping with extra pillows so you are not lying completely flat. You could also temporarily avoid lying on your affected side. When you get up from lying down, try to sit still for a minute to allow any symptoms to settle.
Good sleep is important for recovery. Optimizing your sleep can be key to improving your symptoms, and is an important consideration during rehabilitation.
Wondering if vestibular rehab could help you? Get in touch to speak to one of our physiotherapists!
-
Albathi, M., & Agrawal, Y. (2017). Vestibular vertigo is associated with abnormal sleep duration. Journal of Vestibular Research, 27(2–3), 127–135. [link]
Andrade Junior, M. C. de, Stefanini, R., Gazzola, J. M., Haddad, F. L. M., & Ganança, F. F. (2021). Individuals with peripheral vestibulopathy and poor quality of sleep are at a higher risk for falls. Brazilian Journal of Otorhinolaryngology, 87(4), 440–446. [link]
Aoun, R., Rawal, H., Attarian, H., & Sahni, A. (2019). Impact of traumatic brain injury on sleep: An overview. Nature and Science of Sleep, Volume 11, 131–140. [link]
Besnard, S., Tighilet, B., Chabbert, C., Hitier, M., Toulouse, J., Le Gall, A., Machado, M.-L., & Smith, P. F. (2018). The balance of sleep: Role of the vestibular sensory system. Sleep Medicine Reviews, 42, 220–228. [link]
Byun, H., Chung, J. H., Jeong, J. H., Ryu, J., & Lee, S. H. (2022). Incidence of peripheral vestibular disorders in individuals with obstructive sleep apnea. Journal of Vestibular Research, 32(2), 155–162. [link]
Kim, S. K., Kim, J. H., Jeon, S. S., & Hong, S. M. (2018). Relationship between sleep quality and dizziness. PLOS ONE, 13(3), e0192705. [link]
Micarelli, A., Viziano, A., Pistillo, R., Granito, I., Micarelli, B., & Alessandrini, M. (2021). Sleep Performance and Chronotype Behavior in Unilateral Vestibular Hypofunction. The Laryngoscope, 131(10), 2341–2347. [link]
Petry A, Leuzzi M, Thibault C, et al. High prevalence of sleep disorders in Ménière’s disease: Interplay between vestibular function and sleep. Journal of Vestibular Research. 2025;0(0). [link]